CDC director agrees hospitals have monetary incentive to inflate COVID-19 data

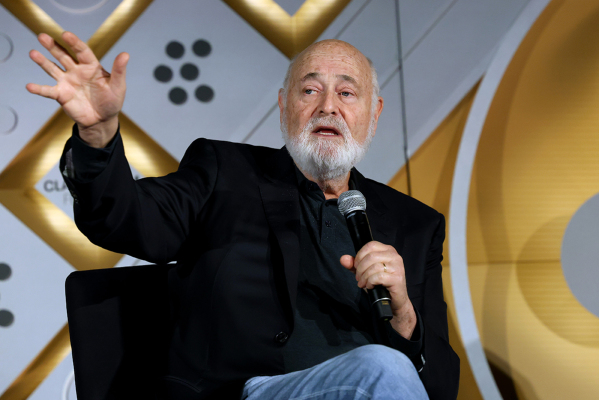
U.S. Centers for Disease Control and Prevention Director Robert Redfield acknowledged during a House hearing Friday that COVID-19 data could be inflated because hospitals receive a monetary gain by reporting COVID-19 cases.
Republican Rep. Blaine Luetkemeyer of Missouri questioned Redfield during a House Oversight and Reform subcommittee hearing on coronavirus containment. He asked about the “perverse incentive” for hospitals to classify deaths as being coronavirus related when the virus didn’t cause the death.
Luetkemeyer voiced concern about how an automobile accident-related death could be recorded as a COVID-related death. In this scenario, the death was recorded as COVID-related because the virus was in the victim’s system, even if the car accident was the major factor.
“As long as you have COVID in your system you get to claim it as a COVID death, which means you get more money as attending physician, hospital, whatever,” Luetkemeyer said during the hearing. “Would you like to comment on that, about the perverse incentive? Is there an effort to try and do something different.”
Redfield responded by telling the congressman, “I think you’re correct in that and we’ve seen this in other disease processes too.”
“In the HIV epidemic, somebody may have a heart attack but also have HIV,” Redfield explained. “The hospital would prefer the DRG [death report] for HIV because there’s greater reimbursement. So I do think there is some reality to that.”
.@RepBlaine Luetkemeyer (R) suggests, without evidence, that US coronavirus deaths are inflated because hospitals are conspiring to get more money
— Aaron Rupar (@atrupar) July 31, 2020
"I think there's some reality to that," responds CDC Director Redfield pic.twitter.com/eSLS1LCvF0
Redfield said that death reporting comes down to what a physician thinks and how he or she classifies a death in a death certificate. He also said the National Center for Health Statistics reviews “all those death certificates.”
“I think it is less operable in the cause of death although I won’t say there are not some cases,” he said. “I do think, though, when it comes to hospital reimbursement issues for individuals that get discharged, there could be some play in that for sure.”
Luetkemeyer previously posed a similar question to Adm. Brett Giroir, Department of Health and Human Services assistant secretary for health, in a July 2 hearing. However, the discussion was halted due to time constraints.
In the July 2 hearing, the legislator also asked about the discrepancy in COVID-19 reporting that saw an automobile death recorded as a COVID-19 death.
“The CDC that gathers the statistics is completely dependent on the reports of the local coroners,” Giroir responded. “Yes, there appear to be some misincentives to over-code.”
On Friday, Luetkemeyer referenced a Colorado study that found COVID-19 reporting data to be inflated.
Earlier this year, the Colorado Health Department reported that nearly a quarter of the coronavirus-related deaths in state statistics did not have the virus listed on their death certificates. The discrepancy caused the state to change the way it reports COVID-19 deaths.
“[Giroir] acknowledges that the statistics he’s getting from the states are inflated,” Luetkemeyer said Friday. “We found that the governor of Colorado, who was a Democrat, actually did research on this and found he had to get rid of 12% of the deaths that were recorded in the state.”
While Luetkemeyer, Redfield and Polis suggest that data shows inaccurately high numbers of COVID deaths, others have come to an opposite conclusion.
A July study by Yale University concluded that there could be substantially more deaths from COVID-19 than reported.
The conclusion came after researchers compared the number of excess U.S. deaths from any cause with the reported number of weekly COVID-19 deaths from March 1 through May 30 using National Center for Health Statistics data.
The numbers were then compared with deaths from the same period in previous years.
“Our analyses suggest that the official tally of deaths due to Covid-19 represent a substantial undercount of the true burden,” Dan Weinberger, an epidemiologist at Yale School of Public Health and a lead author of the study, told CNBC.
Friday’s House panel discussion was titled “The Urgent Need For A National Plan To Contain The Coronavirus.” Subcommittee Chairman Jim Clyburn, D-S.C, discussed hospitals in his remarks and said experts predict 150,000 more Americans could die of the virus at the current rate.
Clyburn contended that hospitals could soon “have to choose who to treat and who to turn home to die.”
President Donald Trump, however, said in a press briefing last Wednesday that the country has made proactive partnerships to “build the greatest medical arsenal in history.”
“We’ve contracted with companies … to produce over 200,000 ventilators by the end of this year, nearly seven times more than we normally would,” the president said. “We’ve contracted … to increase U.S. production of N95 masks.”
The reason for the switch was to obtain more complete and transparent data.
Despite this reasoning, the new database has experienced delays and discrepancies when it comes to the reporting of available hospital beds and ventilators when the exact number for each hospital is crucial, according to NPR.
“If the information is not accurate, it could cost time and lives," Lisa M. Lee, former chief science officer for public health surveillance at CDC, told NPR. "If all the ICU beds are taken up, emergency medical personnel need to take [new patients] to the next town over or to the next county."
Some hospitals have followed the same protocol of sending data for 15 years, then abruptly changed the process on July 10.
Michael Caputo, HHS assistant secretary for public affairs, told NPR that the CDC could not keep up with the old system of reporting data.
Redfield told reporters in mid-July that the CDC agreed to remove the CDC’s National Healthcare Safety Network from the collection process in order to speed up the reporting process.